【协和医学杂志】围术期睡眠质量对术后疼痛的影响研究进展
时间:2024-08-06 12:01:56 热度:37.1℃ 作者:网络
综 述
术后疼痛是围术期常见不良反应,自麻醉学科诞生以来,减轻乃至消除手术带来的医源性疼痛一直是麻醉科医生致力的方向。2013年美国的一项调查表明,约86%的患者术后出现手术相关疼痛,其中75%在住院期间发生中至重度疼痛,且约10%的急性术后疼痛会转化成慢性疼痛[1]。国内相关研究也表明,在接受不同类型的手术后,中至重度急性疼痛发病率可达58.7%[2],而慢性疼痛发病率可达11.3%~43.9%[3-4]。术后疼痛不仅给患者带来不良体验,影响其功能恢复[5],也可导致阿片类药物滥用与医疗负担增加[6]。近年来,越来越多的研究表明,围术期睡眠质量不佳是术后疼痛的一项风险因素[7]。因此,本文就睡眠质量评估、围术期睡眠质量影响术后疼痛的机制以及干预方式等方面展开综述,以期为提升患者围术期疼痛管理水平提供参考。
1 睡眠质量评估
研究表明,我国一般人群中睡眠质量不佳的患病率约为6.6%~18.6%[8-9],在一些高危人群中睡眠质量不佳的发生率会进一步升高,如围绝经期女性可达31.8%[10],而在外科术前患者中可达53.4%[11],且高达87.3%的患者手术当日睡眠质量不佳。
目前,睡眠质量可通过客观检查和主观问卷两种途径进行评估。其中,客观检查主要包括多导睡眠图(PSG)和体动监测(actigraphy),其优势在于能够客观记录受试者睡眠与觉醒的时间,并对睡眠进行分期。而主观问卷由于其便于开展,可评估一段时间内的睡眠质量并反映受试者主观满意度及对日常生活的影响,在临床研究中更为常用。
常见的主观问卷包括匹兹堡睡眠质量指数(PSQI)(表1)、艾普沃斯嗜睡量表(ESS)、失眠严重程度指数(ISI)、利兹睡眠评估问卷(LSEQ)及其他综合性评估量表,如PROMIS(patient-reported outcomes measurement information system)的睡眠部分等。
表1 匹兹堡睡眠质量指数评分表[12]
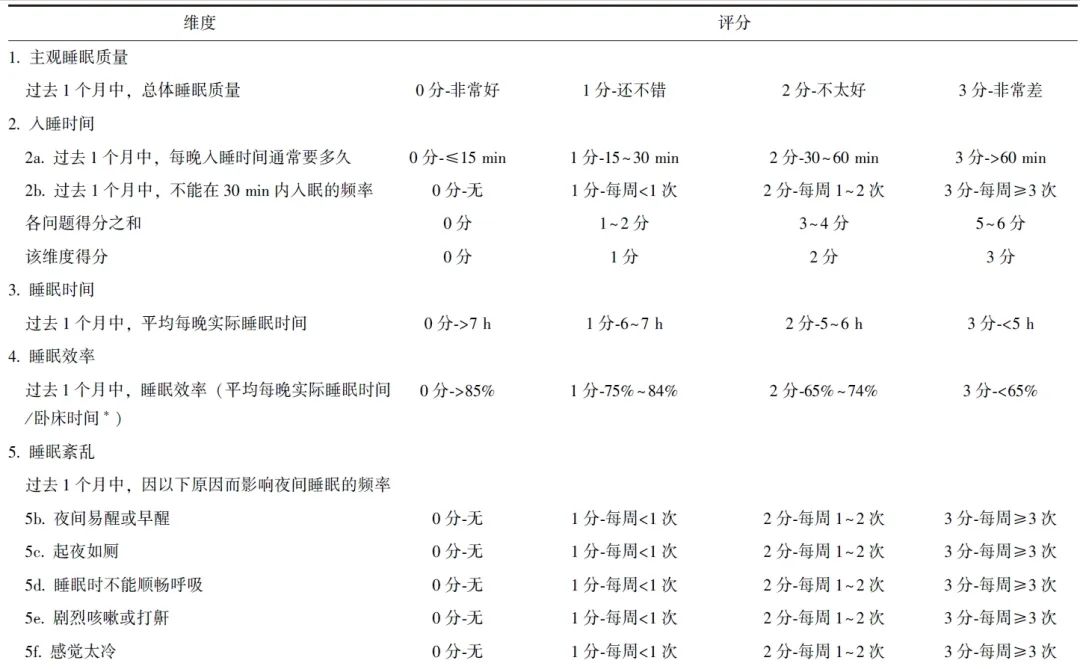
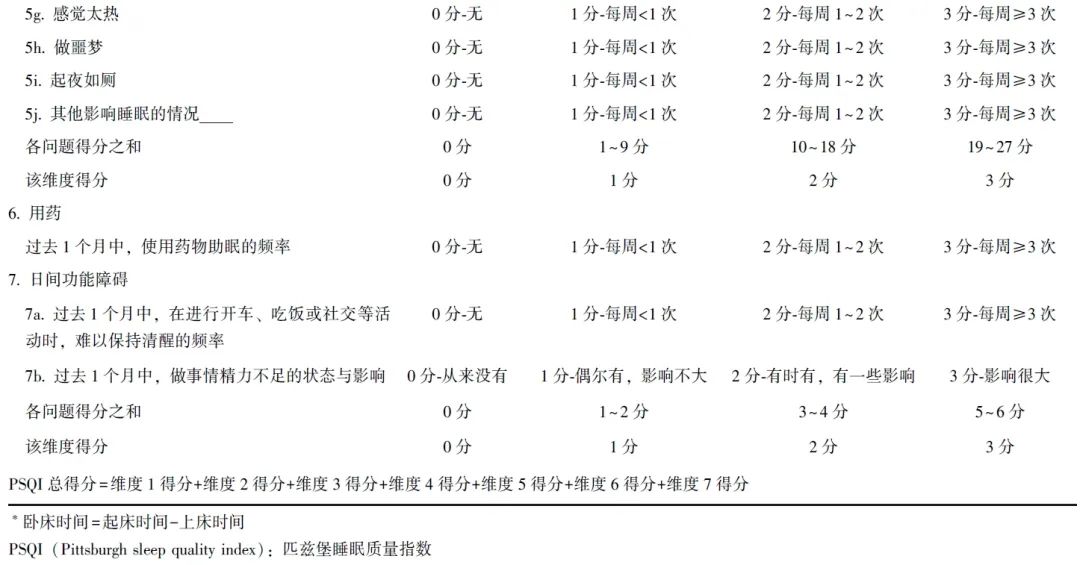
其中,PSQI是目前应用最广泛的睡眠质量评估方法,可评估近1个月内睡眠质量(包括主观睡眠质量、入睡时间、睡眠时间、睡眠效率、睡眠紊乱、用药和日间功能障碍)[12],国外一般以PSQI>5分代表睡眠质量较差,而国内则以失眠人群作为验证数据集,以PSQI>7分代表睡眠质量不佳[13]。
2 围术期睡眠质量与急性术后疼痛
2.1 术前睡眠质量与急性术后疼痛
2019年的一项荟萃分析总结了急性术后疼痛管理不佳的风险因素,其中术前睡眠质量不佳导致患者出现疼痛管理不佳的风险提高了2.3倍,是最重要的风险因素[14]。既往在接受乳腺手术、妇科腹腔镜手术、剖宫产术等的患者研究中也发现,当患者术前1个月的睡眠质量较差时(PSQI>5分),术后24 h内的最高疼痛评分明显增高[15-16]。
在儿科患者群体中,体动监测的术前7 d内平均睡眠时长与术后2周内的急性疼痛程度相关[17]。而在成人保乳手术患者中亦发现术前1 d体动监测的睡眠效率(睡眠时间/卧床时间)是急性术后疼痛的保护因素,但术前1 d单纯睡眠时长与之相比无统计学差异[18],提示对术前一段时间内的睡眠质量评估可能更具价值。
Mamie等[19]对术后疼痛风险因素进行分析发现,术后疼痛与慢性睡眠障碍的相关性较术前2~3 d睡眠质量的相关性更显著,且在62项风险因素中,慢性睡眠障碍为关联度最强的风险因素。然而值得注意的是,上述研究并未评估受试者术后睡眠质量及其对术后疼痛的影响。
2.2 术后睡眠质量与急性术后疼痛
除此之外,也有研究关注了术后睡眠质量与急性术后疼痛的相互作用[20-21],手术刺激不仅会给患者带来疼痛,也会显著影响其术后睡眠质量。有研究表明,术后首日的睡眠结构会发生明显改变,表现为慢波睡眠(SWS)以及快速动眼睡眠(REM)时长的显著减少,且术后2周仍有1/4的患者存在睡眠问题或需睡眠相关治疗[21]。
术后更困倦的患者倾向于体验到更剧烈的疼痛,而因疼痛及镇痛药物导致的入睡困难或睡眠中断又会影响患者的功能恢复,即术后睡眠质量与急性术后疼痛相互影响。因此,对疼痛的干预有助于提升睡眠质量,随着术后疼痛的减轻,患者的睡眠质量可在术后6周至3个月内恢复至术前水平[22]。而对睡眠质量的干预也有助于减轻疼痛,针对骨科患者的研究表明,术后2周内使用唑吡坦(5 mg/d)有助于减轻疼痛,促进患者的功能恢复[23]。
由此可见,术前1周至术后1个月的睡眠质量与急性术后疼痛程度显著相关,而对术后睡眠质量的干预也有助于减轻急性术后疼痛。
3 围术期睡眠质量与慢性术后疼痛
3.1 术前睡眠质量与慢性术后疼痛
根据国际疾病分类编码第11版(ICD-11)[24]的定义,慢性术后疼痛是指术后产生或加剧的、不能被其他原因解释的,且持续时间超过手术切口愈合时间至少3个月的疼痛。研究表明,围术期睡眠质量对急性术后疼痛向慢性术后疼痛转化有一定影响。针对行髋关节置换术和膝关节置换术治疗的患者研究显示,高PSQI评分与慢性术后疼痛相关[25-26]。
另一项针对该群体的研究则表明,高PSQI评分与急性术后疼痛及术后镇痛药用量相关,而与慢性术后疼痛不具有显著相关性[27]。采用PROMIS[28]、mProfile-29[29]及青少年睡眠觉醒量表(ASWS)[30]的研究亦证实,术前睡眠质量与慢性术后疼痛相关。术前睡眠质量与慢性术后疼痛相关性荟萃分析表明,二者存在统计学相关性但效应相对有限[31]。
3.2 术后睡眠质量与慢性术后疼痛
术后睡眠质量与慢性术后疼痛的研究则更倾向于揭示二者的相互影响,针对接受关节手术的患者研究显示,术前及术后6周的睡眠时长均与术后3个月的慢性疼痛相关[32],且术前及术后存在失眠问题的患者倾向于使用更多的阿片类药物,进一步导致睡眠质量恶化[33]。针对接受胸外科手术患者的研究发现,携带PER1基因隐性纯合子的患者围术期睡眠质量较差,更易出现慢性疼痛[34]。
综上,术前睡眠质量与慢性术后疼痛程度可能相关,但效应有限。而术前与术后睡眠质量则与术后镇痛药的用量相关,提示对围术期睡眠质量进行干预是必要的,对于存在慢性睡眠问题的患者,更应重视慢性术后疼痛的管理。
4 睡眠质量影响术后疼痛的分子机制
在健康人群中的睡眠剥夺研究表明,完全睡眠剥夺(TSD)、SWS剥夺以及REM剥夺[又称异相睡眠剥夺(PSD)]均可造成健康人群的温度觉及触觉痛阈下降,而补救性睡眠可在一定程度上减少痛阈下降[35-40],虽然不同研究采用的睡眠干预与疼痛评估方式不同,但睡眠剥夺造成痛阈下降的相关结论相似,而痛阈的改变是否与特定睡眠周期相关仍有待进一步探究。此外,睡眠剥夺也会影响患者的情绪及注意力,进而影响其对疼痛的感知[21]。
采用大鼠睡眠剥夺模型进行痛觉过敏的行为学研究表明,以REM睡眠剥夺模型产生痛觉过敏反应最为明显,其可抑制内源性及外源性阿片类药物的镇痛作用[40]。基于此,研究者对睡眠剥夺影响痛阈的神经生物学机制进行研究发现,睡眠剥夺可引起大鼠脊髓中小胶质细胞激活及神经炎性反应,进而造成痛阈降低及恢复时间延长[41-43]。
此外,背根神经节L-型钙通道过表达与术后痛阈降低时间延长相关[44],术前PSD可通过下调脑源性神经营养因子信号通路加重术后痛觉过敏反应[45],伏隔核与腹外侧中脑导水管周围灰质的功能连接下降及多巴胺能神经元表达下调相关[46]。然而,目前睡眠质量对围术期痛觉过敏影响的作用机制尚未完全阐明,仍有待进一步研究。
5 干预方式
研究表明,围术期使用褪黑素可减轻术后急性疼痛的程度,使术后平均疼痛视觉模拟评分(VAS)下降约1.1分[47-48]。而术前使用唑吡坦(10 mg)可减少术中及术后阿片类药物用量,并使术后首日VAS下降近1分[49]。如在术后患者自控镇痛泵中加入小剂量右美托咪定则有助于提升睡眠质量,同时可减少术后阿片类药物用量,并使术后2 d VAS下降近1.5分[50]。此外,单纯延长2 h睡眠时间亦可减轻急性术后疼痛程度[51]。
针对睡眠质量影响因素进行干预也有助于围术期疼痛管理。
1 对患者面临的压力及环境因素进行干预
研究表明,认知行为治疗(CBT)可提高患者围术期睡眠质量并减轻术后疼痛[52];药物治疗方面,使用艾司西酞普兰对有疼痛灾难化(pain catastrophing)倾向的患者进行干预可减轻术后次日至术后6 d的疼痛水平[53],而在妇科手术患者中使用新型抗抑郁药物艾司氯胺酮也被证实可改善术后睡眠质量和疼痛水平[54]。此外,通过使用眼罩和耳塞改善患者睡眠环境,可减低患者术后首日的睡眠质量下降程度及术后阿片类药物用量[55]。
2 对手术相关因素(如手术创伤、麻醉、药物等)进行干预
其中,手术创伤可显著影响睡眠质量,如腹腔镜手术对睡眠质量的影响要小于开腹手术[56]。与椎管内麻醉相比,全麻对骨科及妇科手术患者的睡眠质量影响更大,而阿片类药物及止吐药物被认为是最重要的影响因素[57-58]。针对关节手术患者围术期睡眠质量的荟萃分析表明,通过提高围术期睡眠的质与量均有助于减轻术后疼痛并减少阿片类药物的使用[59]。因此,局部麻醉将有助于改善患者的睡眠质量,而围术期的多模式镇痛则可减少阿片类药物的用量。
6 小结
围术期睡眠质量不佳,尤其是术前长期睡眠质量不佳,与急慢性术后性疼痛控制不佳相关,且在不同种类手术、不同患者群体中均有一致性。睡眠质量与术后疼痛存在相互作用,然而相关分子机制仍有待进一步阐明。通过提升患者围术期的睡眠质量有助于减轻术后疼痛,提示在临床工作中,应关注患者的围术期睡眠质量,并在必要时对睡眠质量及其影响因素进行干预,以提升患者的围术期疼痛管理水平与恢复质量。
参考文献
[1]Gan T J, Habib A S, Miller T E, et al. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey[J]. Curr Med Res Opin, 2014, 30(1): 149-160.
[2]Zhang Y E, Xu X F, Gong R R. Postoperative pain management outcomes at a Chinese hospital: a cross-pal survey[J]. J Perianesth Nurs, 2023, 38(3): 434-439.
[3]Jin J Y, Peng L H, Chen Q B, et al. Prevalence and risk factors for chronic pain following cesarean p: a prospective study[J]. BMC Anesthesiol, 2016, 16(1): 99.
[4]Zhang Y Y, Zhou R, Hou B L, et al. Incidence and risk factors for chronic postsurgical pain following video-assisted thoracoscopic surgery: a retrospective study[J]. BMC Surg, 2022, 22(1): 76.
[5]Perkins F M, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors[J]. Anesthesiology, 2000, 93(4): 1123-1133.
[6]Glare P, Aubrey K R, Myles P S. Transition from acute to chronic pain after surgery[J]. Lancet, 2019, 393(10180): 1537-1546.
[7]刘星扬, 郭立哲, 王锷. 老年患者睡眠障碍对术后康复影响的研究进展[J]. 中华麻醉学杂志, 2021, 41(7): 888-892.
[8]谷岩, 徐广明, 尹慧芳. 天津市18岁及以上社区人群睡眠质量调查[J]. 中国心理卫生杂志, 2015, 29(3): 199-203.
[9]陈惟义, 周泽文, 刘颖春, 等. 广西35~74岁壮族人群睡眠状况及其影响因素分析[J]. 现代预防医学, 2022, 49(2): 289-294.
[10]赵秋彦, 唐小红, 黄新桥, 等. 围绝经期妇女睡眠质量及影响因素的研究[J]. 中国妇幼健康研究, 2014, 25(5): 752-754.
[11]王玉珠, 柳莹, 姜允琦, 等. 全膝关节置换患者围术期睡眠质量及影响因素分析[J]. 中华关节外科杂志(电子版), 2022, 16(2): 167-173.
[12]Buysse D J, Reynolds C F 3rd, Monk T H, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research[J]. Psychiatry Res, 1989, 28(2): 193-213.
[13]刘贤臣, 唐茂芹, 胡蕾, 等. 匹兹堡睡眠质量指数的信度和效度研究[J]. 中华精神科杂志, 1996, 29(2): 103-107.
[14]Yang M M H, Hartley R L, Leung A A, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis[J]. BMJ Open, 2019, 9(4): e025091.
[15]Wang J P, Lu S F, Guo L N, et al. Poor preoperative sleep quality is a risk factor for severe postoperative pain after breast cancer surgery: a prospective cohort study[J]. Medicine (Baltimore), 2019, 98(44): e17708.
[16]Yao Z W, Zhao B C, Yang X, et al. Relationships of sleep disturbance, intestinal microbiota, and postoperative pain in breast cancer patients: a prospective observational study[J]. Sleep Breath, 2021, 25(3): 1655-1664.
[17]Rabbitts J A, Groenewald C B, Tai G G, et al. Presurgical psychosocial predictors of acute postsurgical pain and quality of life in children undergoing major surgery[J]. J Pain, 2015, 16(3): 226-234.
[18]Wright C E, Bovbjerg D H, Montgomery G H, et al. Disrupted sleep the night before breast surgery is associated with increased postoperative pain[J]. J Pain Symptom Manage, 2009, 37(3): 352-362.
[19]Mamie C, Bernstein M, Morabia A, et al. Are there reliable predictors of postoperative pain?[J]. Acta Anaesthesiol Scand, 2004, 48(2): 234-242.
[20]Kammel J, Messerer B, Avian A, et al. Post-operative sleep quality and pain in children and adolescents[J]. Saf Health, 2015, 1(S1): A4.
[21]Chouchou F, Khoury S, Chauny J M, et al. Postoperative sleep disruptions: a potential catalyst of acute pain?[J]. Sleep Med Rev, 2014, 18(3): 273-282.
[22]Chen A F, Orozco F R, Austin L S, et al. Prospective evaluation of sleep disturbances after total knee arthroplasty[J]. J Arthroplasty, 2016, 31(1): 330-332.
[23]Gong L, Wang Z H, Fan D. Sleep quality effects recovery after total knee arthroplasty(TKA)--A randomized, double-blind, controlled study[J]. J Arthroplasty, 2015, 30(11): 1897-1901.
[24]Treede R D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11[J]. Pain, 2015, 156(6): 1003-1007.
[25]Bjurström M F, Irwin M R, Bodelsson M, et al. Preopera-tive sleep quality and adverse pain outcomes after total hip arthroplasty[J]. Eur J Pain, 2021, 25(7): 1482-1492.
[26]Soni A, Bartling A, Wanigasekera V, et al. Sleep distur-bance is associated with more severe pain and worse outcome following knee replacement surgery in patients with knee osteoarthritis[J]. Br J Pain, 2020, 14(S1): 8-9.
[27]Luo Z Y, Li L L, Wang D, et al. Preoperative sleep quality affects postoperative pain and function after total joint arthroplasty: a prospective cohort study[J]. J Orthop Surg Res, 2019, 14(1): 378.
[28]Schreiber K L, Zinboonyahgoon N, Flowers K M, et al. Prediction of persistent pain severity and impact 12 months after breast surgery using comprehensive preoperative assessment of biopsychosocial pain modulators[J]. Ann Surg Oncol, 2021, 28(9): 5015-5038.
[29]Baeyens M, Neckebroek M, De Paepe A, et al. ESRA19-0235 Screening for psychosocial variables that predict chronic postsurgical pain[J]. Reg Anesth Pain Med, 2019, 44(S1): A234.
[30]Rabbitts J A, Palermo T M, Zhou C, et al. Psychosocial predictors of acute and chronic pain in adolescents undergoing major musculoskeletal surgery[J]. J Pain, 2020, 21(11/12): 1236-1246.
[31]Varallo G, Giusti E M, Manna C, et al. Sleep disturbances and sleep disorders as risk factors for chronic postsurgical pain: A systematic review and meta-analysis[J]. Sleep Med Rev, 2022, 63: 101630.
[32]Walker J, Campbell C, Pejsa M, et al. (350) Pre- and post-operative sleep is associated with post-operative pain and functioning following total knee replacements[J]. J Pain, 2015, 16(4, Supplement): S63.
[33]Rhon D I, Snodgrass S J, Cleland J A, et al. Comorbid insomnia and sleep apnea are associated with greater downstream health care utilization and chronic opioid use after arthroscopic hip surgery[J]. Pain Physician, 2019, 22(4): E351-E360.
[34]Hastie B, Klodell C, Frye R, et al. Tick-Tock...genes working round the clock: associations with sleep and acute and chronic post-thoracotomy pain[J]. J Pain, 2013, 14(4, Supplement): S33.
[35]Eichhorn N, Treede R D, Schuh-Hofer S. The role of sex in sleep deprivation related changes of nociception and conditioned pain modulation[J]. Neuroscience, 2018, 387: 191-200.
[36]Hijma H, Koopmans I, Klaassen E, et al. A crossover study evaluating the sex-dependent and sensitizing effects of sleep deprivation using a nociceptive test battery in healthy subjects[J]. Br J Clin Pharmacol, 2023, 89(1): 361-371.
[37]Roehrs T, Hyde M, Blaisdell B, et al. Sleep loss and REM sleep loss are hyperalgesic[J]. Sleep, 2006, 29(2): 145-151.
[38]Azevedo E, Manzano G M, Silva A, et al. The effects of total and REM sleep deprivation on laser-evoked potential threshold and pain perception[J]. Pain, 2011, 152(9): 2052-2058.
[39]Tiede W, Magerl W, Baumg rtner U, et al. Sleep restriction attenuates amplitudes and attentional modulation of pain-related evoked potentials, but augments pain ratings in healthy volunteers[J]. Pain, 2010, 148(1): 36-42.
[40]Lautenbacher S, Kundermann B, Krieg J C. Sleep deprivation and pain perception[J]. Sleep Med Rev, 2006, 10(5): 357-369.
[41]Huang Y L, Hao J, Yang X L, et al. Pretreatment of the ROS inhibitor phenyl-N-tert-butylnitrone alleviates sleep deprivation-induced hyperalgesia by suppressing microglia activation and NLRP3 inflammasome activity in the spinal dorsal cord[J]. Neurochem Res, 2023, 48(1): 305-314.
[42]Yang H K, Zhang Y F, Duan Q L, et al. Dehydrocorydaline alleviates sleep deprivation-induced persistent postoperative pain in adolescent mice through inhibiting microglial P2Y12 receptor expression in the spinal cord[J]. Mol Pain, 2023, 19: 17448069231216234.
[43]Wei S N, Zhang H, Lu Y, et al. Microglial voltage-dependent anion channel 1 signaling modulates sleep deprivation-induced transition to chronic postsurgical pain[J]. Sleep, 2023, 46(11): zsad039.
[44]Li Q, Zhu Z Y, Lu J, et al. Sleep deprivation of rats increases postsurgical expression and activity of L-type calcium channel in the dorsal root ganglion and slows recovery from postsurgical pain[J]. Acta Neuropathol Commun, 2019, 7(1): 217.
[45]Xue J J, Li H L, Xu Z Q, et al. Paradoxical sleep deprivation aggravates and prolongs Incision-Induced pain hypersensitivity via BDNF Signaling-Mediated descending facilitation in rats[J]. Neurochem Res, 2018, 43(12): 2353-2361.
[46]Guo M M, Wu Y X, Zheng D H, et al. Preoperative acute sleep deprivation causes postoperative pain hypersensitivity and abnormal cerebral function[J]. Neurosci Bull, 2022, 38(12): 1491-1507.
[47]Borazan H, Tuncer S, Yalcin N, et al. Effects of preoperative oral melatonin medication on postoperative analgesia, sleep quality, and sedation in patients undergoing elective prostatectomy: a randomized clinical trial[J]. J Anesth, 2010, 24(2): 155-160.
[48]Andersen L P H, Werner M U, Rosenberg J, et al. A systematic review of peri-operative melatonin[J]. Anaesthesia, 2014, 69(10): 1163-1171.
[49]Xiao Z N, Long B, Zhao Z J. The effect of improving preoperative sleep quality on perioperative pain by zolpidem in patients undergoing laparoscopic colorectal surgery: a prospective, randomized study[J]. Pain Res Manag, 2022, 2022: 3154780.
[50]Chen Z L, Tang R D, Zhang R, et al. Effects of dexmedetomidine administered for postoperative analgesia on sleep quality in patients undergoing abdominal hysterectomy[J]. J Clin Anesth, 2017, 36: 118-122.
[51]Roehrs T A, Roth T. Increasing presurgery sleep reduces postsurgery pain and analgesic use following joint replacement: a feasibility study[J]. Sleep Med, 2017, 33: 109-113.
[52]Yang Y, Zhang H B, Li Y L, et al. The effectiveness of computer-assisted Cognitive Behavioral Therapy (cCBT) for psychological outcomes in patients with laryngectomy: Randomized controlled trial[J]. J Affect Disord, 2022, 300: 59-65.
[53]Lunn T H, Frokjaer V G, Hansen T B, et al. Analgesic effect of perioperative escitalopram in high pain catastrophizing patients after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial[J]. Anesthesiology, 2015, 122(4): 884-894.
[54]Qiu D, Wang X M, Yang J J, et al. Effect of intraoperative esketamine infusion on postoperative sleep disturbance after gynecological laparoscopy: a randomized clinical trial[J]. JAMA Netw Open, 2022, 5(12): e2244514.
[55]Le Guen M, Nicolas-Robin A, Lebard C, et al. Earplugs and eye masks vs routine care prevent sleep impairment in post-anaesthesia care unit: a randomized study[J]. Br J Anaesth, 2014, 112(1): 89-95.
[56]Su X, Wang D X. Improve postoperative sleep: what can we do?[J]. Curr Opin Anaesthesiol, 2018, 31(1): 83-88.
[57]Song Y N, Liu Y J, Yuan Y, et al. Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing hip fracture surgery: a prospective cohort clinical trial[J]. EBioMedicine, 2021, 70: 103490.
[58]Kjølhede P, Langström P, Nilsson P, et al. The impact of quality of sleep on recovery from fast-track abdominal hysterectomy[J]. J Clin Sleep Med, 2012, 8(4): 395-402.
[59]Shen S P, Wang Y J, Zhang Q, et al. Improved periopera-tive sleep quality or quantity reduces pain after total hip or knee arthroplasty: a systematic review and meta-analysis[J]. Orthop Surg, 2021, 13(4): 1389-1397.


